Chronic Obstructive Pulmonary Disease (COPD)
Chronic Obstructive Pulmonary Disease (COPD) is a prevalent and complex respiratory condition that demands a comprehensive and coordinated approach to care.
As front-line healthcare providers, GPs like yourself play a pivotal role in managing patients with COPD. GPs are typically the first point of contact for individuals experiencing symptoms of chronic respiratory conditions. Here we aim to provide you with valuable insights, practical tips, and effective strategies to enhance the diagnosis, care, and well-being of individuals grappling with COPD.
Diagnosis and Assessment:
The first crucial step involves contemplating and verifying the diagnosis of COPD. Due to the symptoms of this condition, it can go unrecognised and subsequently heavily underdiagnosed, or delayed in diagnosis resulting in disease progression. While the primary symptoms of COPD include breathlessness (dyspnoea), chronic coughing, and sputum production, these signs are not specific and tend to develop gradually outside exacerbations. Additionally, individuals with normal spirometry results often report these symptoms. The challenge lies in recognising COPD amidst its nonspecific symptoms - of which are often attributed to lack of fitness, ageing, and other respiratory infections.

It is imperative to actively consider COPD for patients, with risk factors, such as those who:
- Smoke or are exposed to second-hand smoke - there is a close connection between the amount of smoke inhaled and airflow limitation
- Have asthma
- Are frequently exposed to dust, chemicals and fumes from burning fuel
- Have a medical history of respiratory infections
- Have underdeveloped lungs
- Are 40 or older as lung function can deteriorate with age
- Have a particular genetic disorder associated with COPD, such as alpha-1-antitrypsin deficiency
Accurate diagnosis can be further ensured through informed clinical assessment via spirometry. High-quality control standards should be followed in performing this function test. Additionally, considerable levels of subject effort and collaboration is necessary in the effectiveness of spirometry tests. North Brisbane Sleep and Thoracic performs this fundamental test which can assist in COPD detection. See our Spirometry info page here.
Effective Two-Pronged Approach to COPD Management
Effectively dealing with a chronic condition like COPD necessitates a dual-pronged approach. It involves not only foreseeing and proactively addressing potential issues but also reacting promptly when acute challenges arise. This comprehensive management should focus on four key elements:
- Enhancing overall function
- Preventing deterioration
- Cultivating support networks and honing self-management skills
- Effectively handling exacerbations.
As General Practitioners, your role in guiding patients through pharmacological and non-pharmacological interventions is crucial for enhancing their function and quality of life.
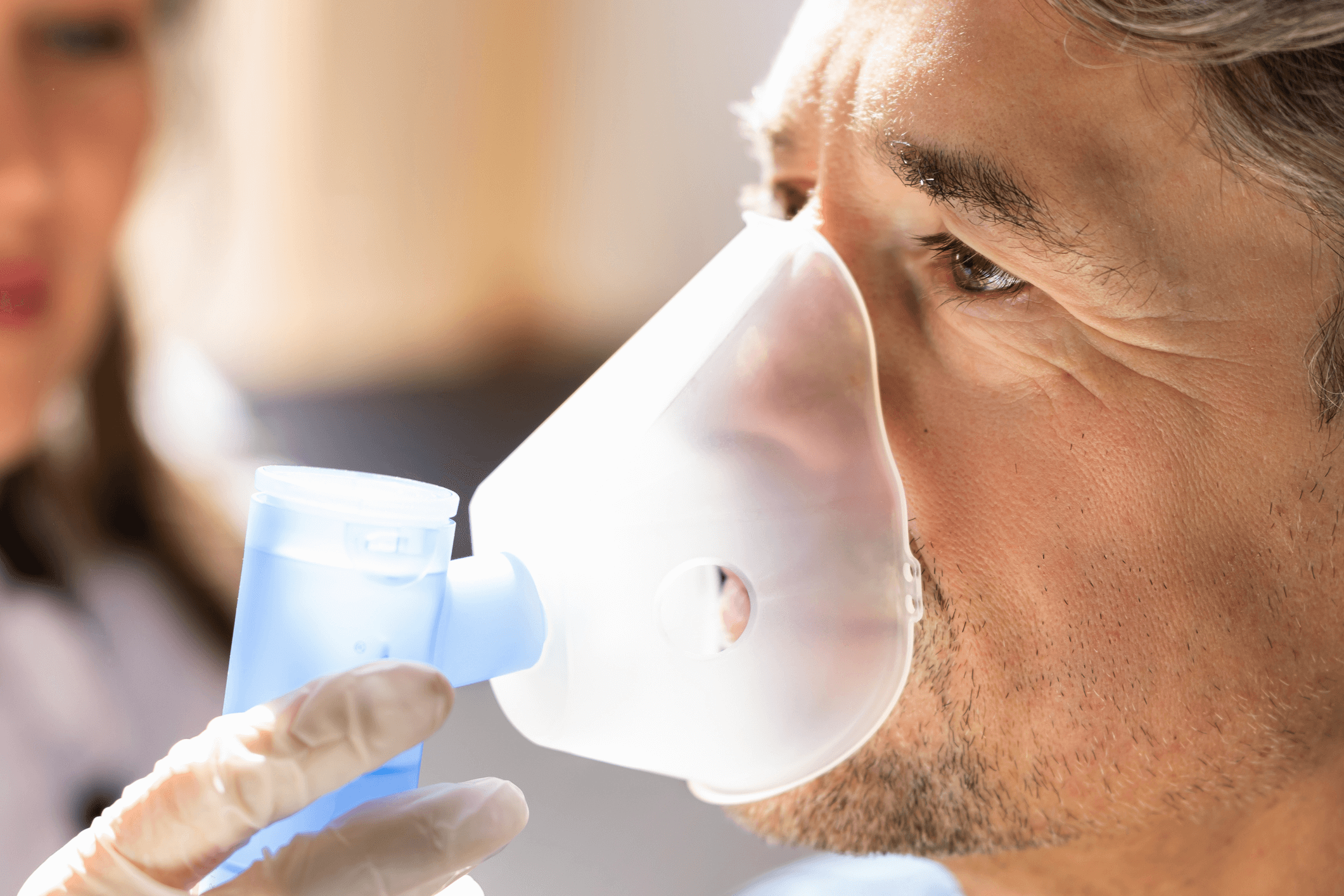
Pharmacological Interventions (Inhaled Medicines)
Through pharmacological methods, patient function can be optimised by decreasing the intensity of exacerbations. Not only can they reduce symptoms but improve the overall health of patient and tolerance to exercise. It's important to note, however, that while these medications offer substantial symptomatic relief, there's currently no evidence supporting their long-term benefits in slowing the decline of lung function. Choosing the appropriate pharmacotherapy requires a nuanced understanding of the patient's disease severity and its impact on their daily life. Regular reviews should be conducted to assess the ongoing benefits and to fine-tune inhaler techniques.
Choosing the appropriate pharmacotherapy requires a nuanced understanding of the patient's disease severity and its impact on their daily life. Yet, assessing the true impact of COPD on an individual extends beyond symptomatic evaluation. It involves understanding the effects on activity limitation, sleep quality, and overall well-being – aspects that might be significantly compromised but not always apparent to healthcare professionals.
Creating a self-management plan for patients in ensuring that they know what to do to manage their condition is an effective method of personalised COPD control. It is essential to forward the patient knowledge on how they can manage their own condition in between GP visits. This should also include an exacerbation plan, with risk-management and recovery techniques to control the flaring up of symptoms. It is important to schedule regular check-ups where you can review the patient's wellbeing and adjust this management plan accordingly, as well as assess their technique and use of inhaler or other pharmacological interventions.
Non-Pharmacological Interventions
Beyond medications, a range of non-pharmacological treatments proves to be highly effective in COPD management. One notable intervention is pulmonary rehabilitation, a holistic program that addresses multiple facets of the patient's condition. This comprehensive approach not only reduces symptoms and disability but also minimises hospitalisation and enhances overall function.
Pulmonary rehabilitation programs typically encompass patient assessment, tailored exercise training, educational components, nutritional intervention, and psychosocial support. While these interventions showcase substantial efficacy, their accessibility may be hindered by resource constraints, geographical limitations, or individual preferences. Acknowledging these barriers is essential, and as GPs, your guidance in navigating these challenges can significantly impact the success of COPD management.
If a patient is a smoker, even a brief counsel urging them to quit this habit can be effective considering the negative impact smoking has on lung function. Influenza and pneumococcal vaccine injections should be scheduled annually to reduce the risk of exacerbations. The overall reduction in risk factors such as the exposure to tobacco smoke, air pollution and other toxin is a helpful intervention. Encouraging patients to exercise regularly within their capability will benefit their health.
Providing education to patients, caregivers, and family members can enhance the timely identification of exacerbations. Collaboratively creating self-management action plans between yourself and North Brisbane Sleep and Thoracic, outlining steps to escalate treatment and enhancing understanding of appropriate responses to deterioration, could prove beneficial.
For information and support and to ensure adequate assistance in COPD management, refer patients to North Brisbane Sleep and Thoracic. Find our contact details here.
Also, see here a resource by the Medical Journal of Australia promoting the "stepwise management" of COPD and the importance of both pharmacological and non-pharmacological interventions.
